Grief is a Journey
What is grief?
Grief, simply put, is the natural and universal emotional response to loss. Feelings of grief include, but are not limited to tearfulness, sadness, difficulty sleeping, anguish, guilt, and anxiety. It is important to understand that grief is a journey that can come in waves, not a state that one simply moves on from. Acute grief occurs in the immediate aftermath of a loss and is characterized by intense pain, sadness, dysphoric emotions, difficulty concentrating, and possible relative disinterest in activities of daily life. This can be distinguished from integrated/abiding grief which is characterized by the deceased easily being called to mind, often associated with longing and sadness. As this journey continues and the loss becomes more integrated into autobiographical memory, thoughts and memories of the deceased are less disabling. It is common during this process for acute grief to “reawaken” at points in time specifically during significant events, holidays, birthdays, anniversaries, or stressful times. You may have heard of the phases of grief: denial, anger, bargaining, depression, and acceptance – this has fallen out of favor because it is too simplistic and limited. While we are giving an overview of grief, this does not describe the full range of feelings accompanying grief. Everyone experiences and perceives things differently and that can affect the way a specific individual experiences grief.
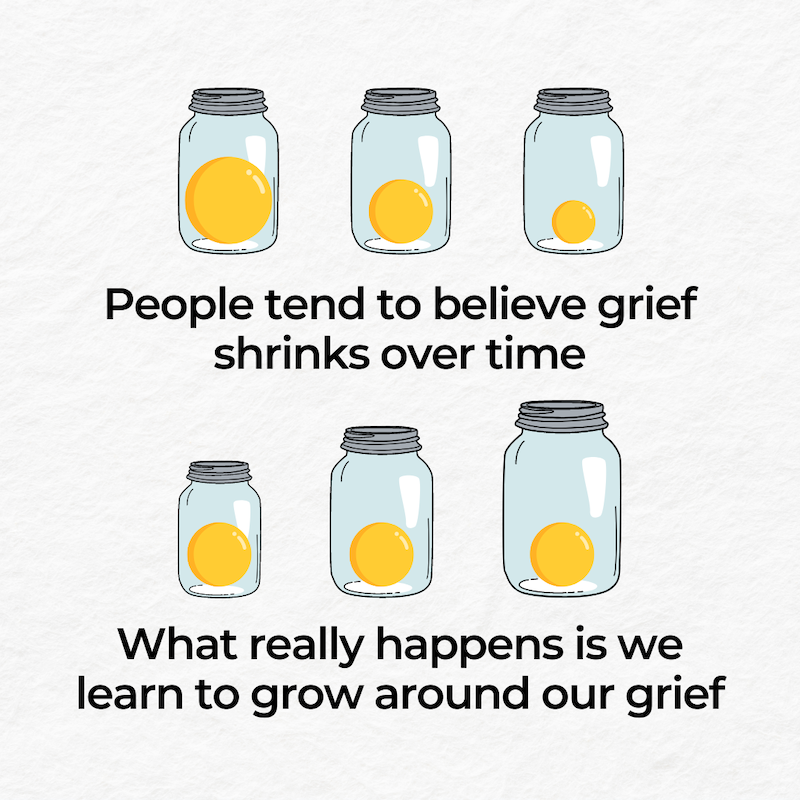
Here is a great image describing the journey of grief:
What is Prolonged Grief Disorder?
Prolonged Grief Disorder is a prolonged grief response lasting longer than 12 months in adults (and longer than 6 months in children) that consistently interferes with daily life. This results from the inability to transition from acute to integrated/abiding grief. Symptoms of this can include intense yearning or preoccupation with thoughts and memories of the deceased occurring most days. Some things that can coincide with this are identity disruption, denial about the death, intense emotional pain, emotional numbness, inability to experience a positive mood, and difficulty reintegrating into relationships and activities. Typically, individuals can progress from acute grief to integrated/abiding grief over 6-12 months, but some individuals may not.
How can I tell if I’m grieving or have Major Depressive Disorder?
Frequently the symptoms of MDD and grief/Prolonged Grief Disorder can overlap, but there are some distinguishing characteristics. A key part of the difference between grief/Prolonged Grief Disorder from MDD is whether thoughts and emotions revolve around the deceased or are more generalized. In Prolonged Grief Disorder, a core symptom is persistent longing for the deceased person whereas with MDD, a core symptom is general anhedonia (lack of interest, enjoyment, or pleasure from life's experiences). Some overlapping features are guilt, isolating behaviors, sleep disturbances, and suicidal ideation.
It’s important to understand that these are not mutually exclusive. There are specific criteria for Prolonged Grief Disorder and MDD and if you are worried about either, we encourage you to reach out to a health professional.
Are there treatments for Prolonged Grief Disorder?
Treatment for Prolonged Grief Disorder is primarily accomplished with “complicated grief therapy.” This type of talk therapy is a combination of cognitive behavioral therapy, interpersonal psychotherapy, and motivational interviewing. This treatment has a dual focus on adapting and coming to terms with the loss and working on a pathway to meaning and satisfaction in life without the deceased loved one. Medications (including antidepressants) can be an additional treatment option if an individual is also suffering from Major Depressive Disorder. As with any mental health diagnosis, coping strategies can help reduce or manage symptoms, such as regular exercise, sufficient quality sleep, balanced nutrition, ecotherapy, mindfulness, and meditation.
The take-home message here is this: Treatment exists for Prolonged Grief Disorder and Major Depressive Disorder, so help is out there. You should always consult with your mental health professional about your treatment plan.
What are common physiologic (aka bodily) changes associated with grief?
Perhaps in contrast to what many may believe, grief can have very real physical effects on the body. Most physiological changes that result from grief or prolonged grief are related to stress. Emotional triggers have been linked to increases in stress hormone release (cortisol), catecholamine release (norepinephrine and epinephrine aka “adrenaline”), and increased sympathetic nervous system stimulation (“fight or flight”). All of this can have effects on your body’s cardiovascular system (heart and blood vessels) such as increased blood pressure and increased heart rate. In rare situations, the sudden loss of a loved one or extreme stressor can result in Takosubo Cardiomyopathy (broken-heart syndrome). Grief and Prolonged Grief can also have more subtle consequences possibly stemming from anhedonia or social isolation. Individuals may be less inclined to address their own healthcare needs and alter their nutritional intake, sleep, and exercise regimens. All of these can have negative impacts on both mental and physical health.
Max’s Story
Nearly four years ago, I lost my father after a long journey with cancer. He was an incredible human, an amazing father, and an even better role model. My journey with grief has not been an easy one – I have endured some of the most stressful times of my life during this process (going through medical school). It took me a long time to move on from the acute grieving process to a more integrated process I think out of fear. I feared that I would start to forget who my father was and how much he meant to me – I felt I would be moving on without him. In the process of transitioning from acute grief to a more integrated grief process, I have needed constant reminders that he is always with me, I will not forget who and what he meant to me, and that he is seeing everything that I am accomplishing right now. Getting into medical school five months after he passed away was an incredibly bittersweet moment. I Facetimed my mom from work and told her the news and while we were both incredibly happy, we had sad tears rolling down our faces. At that moment, I wanted more than anything for my dad to be there to hear this as well. Moments like this, birthdays, holidays, and stressful times often reawaken my acute grief. I cry, I ruminate on thoughts of my dad, I stare at pictures, I watch videos, and listen to music that reminds me of him. Nothing takes away the pain of not being able to share those moments with my father, but it has become a little bit easier with time. I think for me, this has been one of the hardest parts of my grieving process – how can I truly enjoy this moment without being able to share it with him? I often think of a specific moment my mother and I shared with my father a day before he passed – we were helping him get into bed and he had his arms around both of us and started singing a jingle; we all were just giggling in that moment. This is the last memory I have of my father before he peacefully passed away the following day. I share this because ruminating on this memory used to absolutely wreck me. Sometimes it still does but more often than not, I find myself smiling thinking about him just being a goofy guy. Some say that time heals you – grief is not something that you heal from but rather you learn how to process the emotions that come along with it.
My purpose in sharing my story with you is for you to know that grief is not a linear journey. It’s okay to sometimes feel lost during this journey. Grief is not something one gets cured of; it’s something that you live with forever. Sometimes days are tough and sometimes they may be easier. Important moments in your life often can feel bittersweet. For me, having an incredible support network including my mother, sister, brother-in-law, and amazing friends continues to help me throughout this process. I know that there will be future moments such as matching into residency and graduating from medical school where some of this acute grief will reawaken. I have learned to be more compassionate to myself in these moments and allow myself to feel the feelings fully. If you’re reading this, know that grief is a journey.
How to help a friend experiencing grief:
There are many ways to support a grieving friend but one thing that underlies them all is emotional and instrumental (practical aid) support. Some ideas based on a 2021 study on grief support that were shown to be impactful are outlined below:
Acts of emotional caring: Remembering the person who died, speaking their name, sharing memories, acknowledging important dates and holidays, and emotionally sensitive language
Emotional support: Being present, allowing the expression of grief, listening, being available, devoting time, being open to grief emotions, not trying to fix or rush grief, refraining from unsolicited advice, timeless support
Instrumental support: Assistance with childcare, meals, financial support, yard work, housekeeping, written notes, gifts
Here’s what people who have experienced grief want you to know:
“As I continue to navigate the aftermath of losing my friend, I have learned each person's grief journey is unique, and it's okay to experience ups and downs.”
- Jane D. (Syracuse University)
“Know that it is okay to not be okay and no one should judge you for that. Always remember that there is power in being vulnerable and strength in talking about your emotions.”
- Lara S. (Syracuse University)
“To love someone is never a burden, and if grief is unexpressed love, then grieving someone is never a burden either.”
- Julia P. (University of Virginia)
“Grief is not the enemy, rather the price we pay for loving so deeply”
- Katie G. (Clemson University)
Should I go to therapy or counseling for grief?
There is no right answer to the question because grief is very individualistic. Many factors are involved in coping with the loss of someone, such as previous state of mental health, support network, understanding of coping strategies, etc. If you feel that you are struggling with grief, it is okay to reach out and see if grief counseling may be able to help. You can always try it and see if it helps.
Where should I go for help with Prolonged Grief Disorder or MDD:
Your primary care physician (these are typically doctors specializing in Family Medicine or Internal Medicine)
A psychiatrist (a doctor specializing in Psychiatry)
A psychologist (a mental health provider with a PhD or PsyD degree), therapist, or grief counselor (note that these providers cannot prescribe medications but can provide valuable interventions such as therapy)
When should I go to the doctor?
If any of your symptoms cause you distress or impair your day-to-day functioning.
Any thoughts of suicide should prompt emergency treatment. Please call/see your physician, call 988, or visit your local emergency department if you have any thoughts of suicide.
When in doubt, see a healthcare provider or mental health professional. They can help you determine if your symptoms can be helped with mental health treatment, or help you get connected with counseling/therapy.
How do I find a provider that takes my insurance/form of payment?
Visit your insurance provider’s website and locate the provider finder page. This should assist you in finding care in your area that accepts your insurance.
Call your insurance provider to have them assist you in finding a provider in your area.
Use FindTreatment.gov.
See “Mental Health Providers: Tips on Finding One” for more tips and suggestions.
Where can I learn more?
National Alliance on Mental Illness, Personal Story about Grief
Wondermind, Grief Archives
WHAT PEOPLE experiencing grief HAVE TO SHARE WITH YOU:
Published: March 23, 2023.
Written by Max Smith (Medical Student), Edited by Alexandra Lawlor (Medical Student).
References:
Mughal S, Azhar Y, Mahon MM, et al. Grief Reaction and Prolonged Grief Disorder. [Updated 2023 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507832/
Zisook S, Shear K. Grief and bereavement: what psychiatrists need to know. World Psychiatry. 2009 Jun;8(2):67-74. doi: 10.1002/j.2051-5545.2009.tb00217.x. PMID: 19516922; PMCID: PMC2691160.
American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association Publishing. https://www.psychiatry.org/psychiatrists/practice/dsm
Prigerson HG, Shear MK, Reynolds CF. Prolonged Grief Disorder Diagnostic Criteria—Helping Those With Maladaptive Grief Responses. JAMA Psychiatry. 2022;79(4):277–278. doi:10.1001/jamapsychiatry.2021.4201
Kristensen P, Dyregrov K, Dyregrov A. CLINICAL REVIEW Narrative review articles based on the author’s own experience and a discretionary selection of articles. Clinical review What distinguishes prolonged grief disorder from depression? 538 -40. Tidsskr Nor Legeforen nr. 2017;137:538-578. Accessed February 11, 2024. https://tidsskriftet.no/sites/default/files/pdf2017--538-9eng.pdf
Ahmad SA, Brito D, Khalid N, et al. Takotsubo Cardiomyopathy. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430798/
Stroebe M, Schut H, Boerner K. Cautioning Health-Care Professionals. Omega (Westport). 2017 Mar;74(4):455-473. doi: 10.1177/0030222817691870. PMID: 28355991; PMCID: PMC5375020.
Cacciatore J, Thieleman K, Fretts R, Jackson LB. What is good grief support? Exploring the actors and actions in social support after traumatic grief. PLoS One. 2021 May 27;16(5):e0252324. doi: 10.1371/journal.pone.0252324. PMID: 34043716; PMCID: PMC8158955.































If you’re reading this, grief takes time, but so does growth.