Physician Burnout
On the topic of burnout: If you’re a busy student or clinician, but still interested in this topic, we’ve included a short list of six important takeaways at the end.
Is It as Serious as the Media Claims?
In 1973, the United States issued a congressional report titled America Burning. The report described the national impact of structure fires—$11 billion in resources destroyed annually, upwards of twelve thousand killed, and tens of thousands maimed or scarred. One year later, the Federal Fire Prevention and Control Act of 1974 was passed, emphasizing fire prevention. Fast forward 50 years, and the number of fires and injuries has halved, saving billions of dollars and, more importantly, hundreds of thousands of lives. (1)
While fires no longer claim nearly as many lives in the United States, America continues to burn in the wake of COVID-19 and a fragmented healthcare system. Since 2018, there has been a 32% increase in healthcare worker burnout. (2) In recent years, the AMA has recorded record high rates of burnout exceeding 50% in Emergency Medicine, Family Medicine, Internal Medicine, Pediatrics, and OB/GYN. (3) Furthermore, many physicians who acknowledge feelings of burnout and depression will not seek help for various reasons, including fear of retribution from local and state bodies, negative perceptions from peers, and the attitude of "burnout seen as weakness." (4)
Burnout among physicians has been shown to be associated with a six-fold increased risk in medical errors and increased suicidality—40% greater for male physicians and 130% greater among female physicians. (5) The Harvard Gazette estimates that the cumulative annual fiscal impact of physician burnout exceeds $4 billion, which is more likely than not an underestimate. (6)
The concept of burnout is not new for 21st-century medical students, residents, or physicians. The question remains: What is there to do? How do I protect myself? What can I do to support my peers?
What is Burnout?
According to the World Health Organization (WHO), burnout is a syndrome that results from unsuccessfully managed chronic workplace stress. It is commonly characterized by
energy depletion or exhaustion
increasing mental distance from one’s job, or having feelings of negativism or cynicism related to one's job
reduced professional efficacy. (7)
When does Burnout begin?
Unfortunately, burnout can begin long before doctors even start practicing medicine. Studies show that 28-45% of medical students experience burnout during their training, and 27.2% report dealing with depression. Yet, only 15.7% of those students actually seek help. (8)
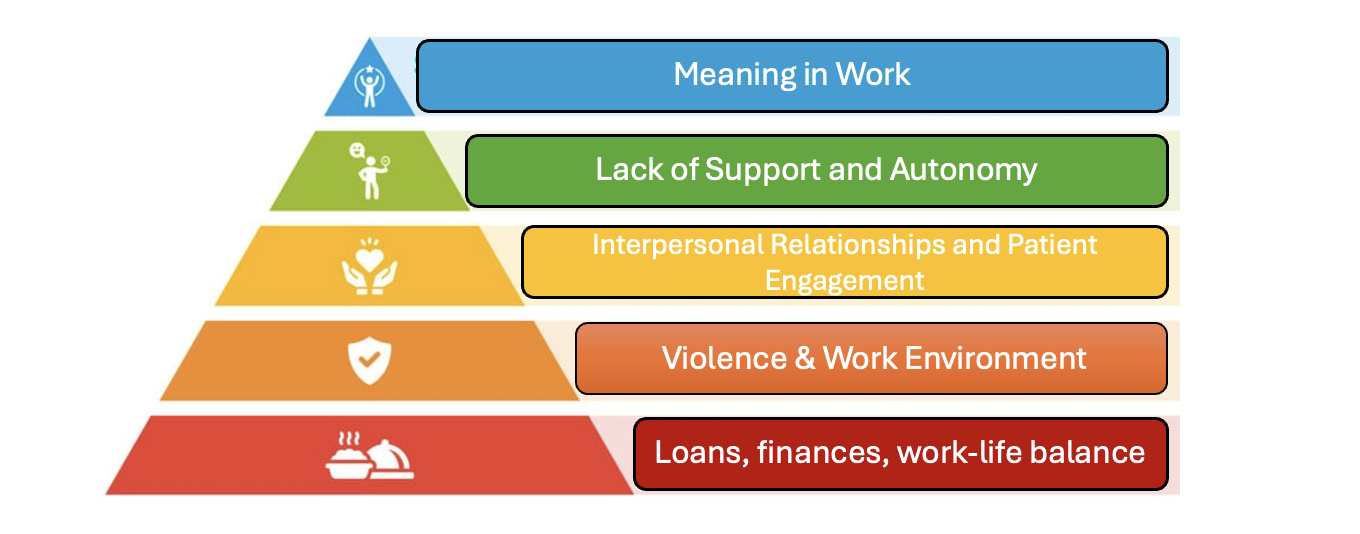
Residents (doctors in training) are also heavily affected, with 27-75% reporting burnout, depending on their specialty. (8-9) When asked what causes burnout, they pointed to several factors, like struggling to maintain a healthy work-life balance, feeling unsupported, and lacking control over their work. (10)
The figure below uses Maslow’s hierarchy of needs to explain how burnout can happen. (10)
What Causes Burnout?
What can I do to prevent or combat burnout?
There is no simple solution, and it would be naive to suggest an elixir to cure burnout exists. Literature does support that institutional change may be appropriate interventions to reduce burnout. (11) However, these interventions will require institutional buy-in and change and will likely take years to implement.
However, after interviewing a small pool of healthcare workers and reviewing the literature, I believe there are small, manageable actions individuals can take to improve mental health and the system at large.
Dr. Benjamin Doolittle and colleagues at Yale University discuss the term eudaimonia—human flourishing—in the context of clinical training. (12) They interviewed training physicians on what factors contributed to thriving at work and more generally in life, noting several core themes: leadership, climate, connectedness, joy in medicine, balance, and various intrinsic factors were central to trainee thriving.
What I have taken away from the literature, Doolittle’s work, and conversations with practicing clinicians is— unsurprisingly—that both our internal perspectives and our external circumstances influence well-being. Unfortunately, we may not be able to influence our circumstances, but we can attempt to control our perspective by asking ourselves what gives purpose, joy, and fulfillment in life and how a vocation in medicine fits into that narrative.
The journey is different for everyone, but that does not mean it is one taken alone. Community is paramount in mitigating burnout; find a trusted friend or colleague who understands the journey and engage in vulnerable conversations about the good days, the bad days, the complex cases, and the comical circumstances. These relationships will not only help you find eudaimonia, but will also build a lifeline for the low times in your career.
Such conversations and perspective-building are preventive, as is engaging in daily physical activity. Even as little as 25-30 minutes can have significant beneficial impacts on mitigating burnout. Similarly, taking time to rest the mind through meditation or practicing mindfulness has been shown to lower burnout among trainees and improve satisfaction at various stages of training. Most important, however, is prioritizing sleep whenever possible.
All of these may sound like no-brainers, but self-care is often the first thing to go when life and schedules get busy. Yet, if we are unable to take care of ourselves, we will be unable to care for patients the way we want to. By actively addressing burnout through self-care, organic grassroots community support, and mindful practices, we can create a more sustainable and fulfilling career in medicine.
6 Takeaways to remember:
Burnout Has Skyrocketed Since 2018 – There has been a 32% increase in healthcare worker burnout, with rates exceeding 50% in several major specialties (Emergency Medicine, Family Medicine, Internal Medicine, Pediatrics, and OB/GYN).
Burnout Directly Affects Patient Care – Physicians experiencing burnout have a six-fold increased risk of making medical errors, which has serious implications for patient safety.
Higher Suicide Risk for Physicians – Burnout is linked to a 40% greater suicide risk in male physicians and a 130% greater risk for female physicians.
Burnout Starts Early – Even before practicing medicine, 28-45% of medical students and 27-75% of residents report burnout. However, only 15.7% of students seek help, often due to stigma and fear of repercussions.
Massive Financial Costs – The estimated annual fiscal impact of physician burnout is over $4 billion, likely an underestimate.
Community is a Key Protective Factor – Having a trusted colleague or friend to discuss both the good and bad days can help prevent burnout and contribute to eudaimonia (human flourishing).
Resources:
American College of Physicians, Individual Physician Wellness and Burnout Tools
American Medical Association, EdHub
American College of Emergency Physicians, Wellness Section
988 Lifeline, Call or text 988, or visit online to chat
WHAT medical Students & Physicians HAVE TO SHARE WITH YOU regarding Mental health:
Published: March 14, 2025.
Written by Joseph L. Williams, MPH (Medical Student), Edited by Alexandra Lawlor, MPH (Medical Student) and Max Smith, MS (Medical Student).
References:
Lessons from Fire Prevention: Why We Can Head Off Disease Without Sacrificing Cure | SPH. Accessed November 17, 2024. https://www.bu.edu/sph/news/articles/2017/lessons-from-fire-prevention-why-we-can-head-off-disease-without-sacrificing-cure/
CDC. Health Worker Mental Health Crisis. Centers for Disease Control and Prevention. October 24, 2023. Accessed November 17, 2024. https://www.cdc.gov/vitalsigns/health-worker-mental-health/index.html
These 6 physician specialties have the most burnout. American Medical Association. August 29, 2023. Accessed November 17, 2024. https://www.ama-assn.org/practice-management/physician-health/these-6-physician-specialties-have-most-burnout
Battling physician burnout one inappropriate form at a time. American Medical Association. November 17, 2023. Accessed November 17, 2024. https://www.ama-assn.org/practice-management/physician-health/battling-physician-burnout-one-inappropriate-form-time
Kalmoe MC, Chapman MB, Gold JA, Giedinghagen AM. Physician Suicide: A Call to Action. Mo Med. 2019;116(3):211-216.
Harvard Gazette. Doctor burnout costs health care system $4.6 billion a year, Harvard study says. Harvard Gazette. July 12, 2019. Accessed November 17, 2024. https://news.harvard.edu/gazette/story/2019/07/doctor-burnout-costs-health-care-system-4-6-billion-a-year-harvard-study-says/
Burn-out an “occupational phenomenon”: International Classification of Diseases. Accessed November 17, 2024. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of Depression, Depressive Symptoms, and Suicidal Ideation Among Medical Students: A Systematic Review and Meta-Analysis. JAMA. 2016;316(21):2214-2236. doi:10.1001/jama.2016.17324
Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236-242. doi:10.4300/JGME-D-09-00054.1
Underdahl L, Ditri M, Duthely LM. Physician Burnout: Evidence-Based Roadmaps to Prioritizing and Supporting Personal Wellbeing. J Healthc Leadersh. 2024;16:15-27. doi:10.2147/JHL.S389245
Physician Burnout. Accessed November 17, 2024. https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
Hyman JH, Doolittle B. Thriving in Residency: a Qualitative Study. J Gen Intern Med. 2022 Jul;37(9):2173-2179. doi: 10.1007/s11606-022-07504-6. Epub 2022 Jun 16. PMID: 35710670; PMCID: PMC9202965. - Google Search. Accessed November 17, 2024. https://www.google.com/search?q=Hyman+JH%2C+Doolittle+B.+Thriving+in+Residency%3A+a+Qualitative+Study.+J+Gen+Intern+Med.+2022+Jul%3B37(9)%3A2173-2179.+doi%3A+10.1007%2Fs11606-022-07504-6.+Epub+2022+Jun+16.+PMID%3A+35710670%3B+PMCID%3A+PMC9202965.&oq=Hyman+JH%2C+Doolittle+B.+Thriving+in+Residency%3A+a+Qualitative+Study.+J+Gen+Intern+Med.+2022+Jul%3B37(9)%3A2173-2179.+doi%3A+10.1007%2Fs11606-022-07504-6.+Epub+2022+Jun+16.+PMID%3A+35710670%3B+PMCID%3A+PMC9202965.&gs_lcrp=EgZjaHJvbWUyBggAEEUYOTIHCAEQIRiPAjIHCAIQIRiPAjIHCAMQIRiPAtIBBzMwMmowajeoAgCwAgA&sourceid=chrome&ie=UTF-8































If you’re reading this, there is a time and season for everything.